From sample donors to new diagnostics

Putting people at the heart of sample collections
From sample donors to new diagnostics: part I

Breakthroughs in diagnostics wouldn’t be possible without people willing to donate biological samples to support research and product development. But researchers start thinking about sample donors far before collections begin.
Behind the scenes, a meticulous process culminates in the creation of a research protocol that defines the research objectives, justifies the collection, ensures an ethical process, protects the rights, safety, and welfare of participants and much more. And only once an institutional review board, including an ethics committee, approves this protocol can collection finally start.
Collecting samples for schistosomiasis
 Principal investigators like Prof. Sammy Njenga have mastered this process in the pursuit of developing life-saving diagnostics for some of the world’s poorest populations. As Chief Research Scientist at the Kenya Medical Research Institute (KEMRI), he is currently leading field studies in Kenya for the evaluation of a rapid diagnostic test that is being developed by FIND and other partners and could revolutionize testing for schistosomiasis, a parasitic disease that affects over 200 million people, mostly in tropical countries.
Principal investigators like Prof. Sammy Njenga have mastered this process in the pursuit of developing life-saving diagnostics for some of the world’s poorest populations. As Chief Research Scientist at the Kenya Medical Research Institute (KEMRI), he is currently leading field studies in Kenya for the evaluation of a rapid diagnostic test that is being developed by FIND and other partners and could revolutionize testing for schistosomiasis, a parasitic disease that affects over 200 million people, mostly in tropical countries.
Current testing for schistosomiasis relies on microscopic examination of stool or urine samples to detect parasite eggs. It involves a complex process, requiring the transfer of samples to a lab and highly skilled staff to interpret the results, making it challenging to deploy testing in community settings. Yet accurate tracking and mapping of cases is imperative to deliver treatments where they are needed and end the scourge of this disease.
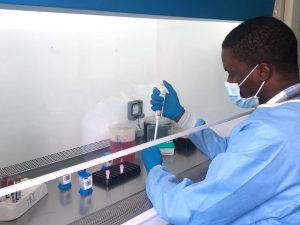
All that may change, however, with diagnostic innovation. With support from project partners, Prof. Njenga and his team are evaluating the performance of a new rapid, point-of-care test that uses a finger stick blood sample. The development of this test has mainly been done using frozen blood samples, but demonstrating its performance in real-life settings, would not be possible without collecting fresh blood samples from affected communities, as well as urine and stool samples for comparative analysis against currently used diagnostics. FIND provided support to collect these well-characterized samples, now stored in KEMRI’s biobanking facility and to conduct the field evaluation studies in schistosomiasis endemic and non-endemic areas of Kenya.
Engaging communities on the journey
Engaging communities well in advance of the actual sample collection and testing is a critical step in the process for informed participation and to inspire participation. Research teams often seek the support of influential decision-makers and trusted community leaders to generate awareness and support for research.
As Prof. Njenga explains, “Clear and transparent communication is key. Most people accept to donate their samples when they understand the clear benefit to them and the community. Participation empowers people to know their health status and receive treatment after a positive test for schistosomiasis, while contributing to a project that can help millions worldwide.”
Ensuring quality collections with tech
Although Kenya is a resource-limited environment with many logistical challenges, collections still abide by high-quality standards. “Our research team followed all the strict procedures for collection, handling, disposal, and storage to ensure the safety of participants and researchers, and the biological integrity of the samples themselves.”
The team also used digital tools to enhance their effectiveness. “Each sample was assigned a unique barcode, which both guarantees anonymity and records key information, including the age and gender of the donor and the date of collection.”
Only part of these precious samples will be used to test the performance of the new fingerstick test. The leftovers will be carefully stored to extend their impact beyond this specific project. “We will continue to work with partners so that these samples can contribute to the development of new diagnostics and treatments. Collaboration is fundamental to bringing us closer to schistosomiasis elimination and saving lives” says Prof. Njenga. Thankfully for those at-risk, his team is as relentless as the disease in this pursuit.
Storing a treasure trove of data
From sample donors to new diagnostics: part II

Following collection, the next stage in the journey to new diagnostics is critical to the integrity of the samples and their value to research and development. A simple misstep could compromise their quality and render them unusable – or, worse still, negate the validity of research down the line. For this reason, they must be transferred to a specialized facility, where experienced scientists will take meticulous care to process and store them.
Going inside a biobank
 The Biobanque de Picardie is one of many such facilities dedicated to the storage of biological samples. “Every sample is a treasure trove of clinical data,” says Yves-Edouard Herpe, Head of Biological Resource Center, “but only if handled correctly.”
The Biobanque de Picardie is one of many such facilities dedicated to the storage of biological samples. “Every sample is a treasure trove of clinical data,” says Yves-Edouard Herpe, Head of Biological Resource Center, “but only if handled correctly.”
Dr Herpe and his team take the raw material – whether leftover from diagnostic analysis or collected for a specific project – and carefully log its origin and characteristics along with other data, for example the donor’s age and any medical conditions. This process turns the samples into a valuable commodity that can be used for research and product development.
One of the first European biobanks to begin operations in 1991, Biobanque de Picardie now stores around 500,000 samples from 50 collections for multiple diseases. Every sample must undergo rigorous quality control checks, processing, and characterization before being carefully registered and stored at optimum temperature.
Quality processing, in practice
“Processing must be carried out in a carefully standardized way to ensure consistent quality across the samples. For this reason, our specialists always work in pairs to prevent any handling or data-entry errors,” says Herpe. Along the journey, traceability is key. “Every step and potential nonconformities that could impact future analyses are thoroughly documented,” he adds.
This level of precision is fundamental to research and product development, with samples used to investigate mechanisms of diseases as well as to test and validate new diagnostics and therapies. Stored carefully, batches can be used in multiple studies. Institutions that hold samples are able to collaborate with academics, nonprofits and the private sector to maximize the impact of samples and become a driving force behind diagnostic test development.
Making the most of a sample
For Herpe, facilitating such diverse research makes all the painstaking effort worthwhile. “It’s immensely satisfying to see samples exit the biobank,” he says, “because we know they’re contributing to the development of new treatments, diagnostics, and vaccines.”
This was certainly the case in the early stages of the COVID-19 pandemic when samples became a prized commodity in the struggle to develop tests. “Despite the number of daily infections reported, it was difficult for diagnostic manufacturers to find ethically collected samples from infected patients,” says Herpe. “We were able to supply leftover samples to help the researchers validate their tests with the speed required.”
In January 2021, the facility also contributed to EpiCov, the largest French epidemiological study on COVID-19 to evaluate the immunity status of the population – yet another powerful example of the role human samples are playing in advancing diagnostics and healthcare today.
Unlocking the value of biological samples
From sample donors to new diagnostics: part III
The last step of the sample journey is also the beginning of a new path toward scientific discovery. A diagnostic developer has designed an experiment, but needs a specific set of biological samples to start. The developer must rely on a process that until now, has involved many stakeholders in a complex choreography.
For the results of this experiment to be relevant, samples used must be high-quality, supported by good clinical data and come from the test’s intended populations and settings (usually originating from donors in different countries).
The evaluation of the resulting diagnostic test’s performance will depend on these crucial samples—but whether this diagnostic developer, or any other researcher, can access them is a different matter. A primary challenge that stands in the way is funding.
Diagnosing the funding dilemma
 Dr Jayne Sutherland recently found herself confronting this funding issue. As Associate Professor of Immunology and Head of Tuberculosis (TB) Research Group at MRC Unit The Gambia at LSHTM, Dr Sutherland is working on developing a rapid diagnostic test (RDT) for TB triaging that could better diagnose and ultimately help treat millions of people each year affected by TB, mostly in low- and middle-income countries. Like many other researchers, she faced a dilemma.
Dr Jayne Sutherland recently found herself confronting this funding issue. As Associate Professor of Immunology and Head of Tuberculosis (TB) Research Group at MRC Unit The Gambia at LSHTM, Dr Sutherland is working on developing a rapid diagnostic test (RDT) for TB triaging that could better diagnose and ultimately help treat millions of people each year affected by TB, mostly in low- and middle-income countries. Like many other researchers, she faced a dilemma.
“We’ve identified a promising biomarker signature for TB in samples collected in Gambia. Our main challenge has been to validate it in global samples so that we can get the funding to develop our lab-based test into one that’s suitable for primary healthcare settings.” Dr Sutherland explained. “But without funding to prospectively collect samples in other countries, we haven’t been able to reach this milestone.” All this changed in June 2021.
Stored samples: a cost-effective solution
With the help of stored TB samples from the FIND Specimen Bank collected in Africa, Latin America, and Southeast Asia, Dr Sutherland was able to solve this ‘chicken-and-egg’ paradox and resume test development.
“Although we don’t know the results yet, the ability to access well-characterized multi-origin samples is very valuable to us and far cheaper than running our own collection,” she said. This means the MRC Unit is one step closer to producing a vital and affordable point-of-care rapid diagnostic test (RDT) enabling more people to be screened for TB.
Collaborating to extend the impact
Better access to samples can improve potential partnerships with other diagnostic developers. The MRC unit, for instance, collects far more samples than its team alone can analyse and Dr Sutherland emphasizes they are “more than happy for other researchers to access them if it contributes to new diagnostics, vaccines, or medicines that can ultimately help more patients.” The key, she says, is to ensure that sample-collecting institutions are acknowledged and that benefits are shared through collaboration.
When researchers enjoy facilitated access to stored samples it advances product development, validates results at a lower cost, and forges the way toward positive results in infectious disease control around the world.
FIND Biobank services foster the ethical collection of and efficient access to samples to support research and streamline the diagnostic development process. More on FIND Biobank services.

